Following up from my last post, our darling little boy has arrived!
Eizac Chen Kai En – God’s special delivery to our home.
His birth story is not as eventful as his older brother’s (thankfully) but quite an experience by itself. Before my post-delivery cotton brains become more fluffy; here goes the story:
30th January 2013; 9am
It was Week 37 + 3 days of gestation for Baby Eizac. I had the next week planned out before the scheduled caesarean on 6th Feb 2013. There were a million and one more things to complete before Baby Eizac’s arrival. With the pending Chinese New Year festival season; we were trying to get ready for the festive days; settle Xi En into his not-so-new school + get ready the house & resources for Eizac’s arrival.
I drove Xi En to school at 9am and my mum decided to take the day off to visit my nephew in the west.
10:30am
Cleared most of my work-related matters. Passed some documents and keys to my colleague who drove by to take over my work. Settled down at home to finish up on my Korean drama serial. Last few episodes to go; best to finish up before my life is all about washing milk bottles; breastfeeding; soiled diapers and more soiled diapers. 😛
12-2pm
Had my lunch. I recalled it was instant noodles. Was hungry again at 130pm. Ate some chips and chocolates. Finally full by 2pm.
Decided to nap at 2pm. Such luxury is only reserved for the heavily pregnant. 🙂 Before I could even lie down on the bed, I felt a gush of discharge. Experience tells me it’s not too good.
Quick check in the loo to discover a river of unstoppable bleed.
That’s it – I told myself. Eizac must have decided to go heads on with the placenta!
It was a moment of panic. I was A.L.O.N.E at home. The hospital bag which was meant to be packed is still somewhere in my head.
I don’t want to be delivering my baby at home!
Breathe-in; Breathe-out; I told myself. Think straight. Yes – In & Out; In & Out (no, not the burgers!)
While trying to stop the bleed; I called 995. Amidst my panicky voice, I managed to tell the operator my address and explained the situation.
And amazingly; I managed to grab a bag and threw in most of the essential stuff which I might need (told you the hospital bag was “in my head”).
Called Kim next and told him baby’s on his way!
Sent a SMS to my obstetrician next. I was so worried that she wasn’t back from her travels. She did highlighted that she was travelling during the week and I wasn’t sure if she was back in town. Thankfully, she replied almost immediately to say she will see me directly at the delivery suite. Phew… it was a huge relief to know that my trusted obstetrician will be delivering Eizac.
210pm
Ambulance arrived with the paramedics in 10 mins flat. I managed to lug the bag, my tummy and myself to the door. The paramedics asked me to get onto the stretcher (propped in a sitting position).
I told them I need to lock the doors first because no one is at home. I wasn’t thinking straight I think. They scolded me and told me they will lock up. Asked me to get on asap.
Errm.. I forgot I called for help, hey. :S
230pm
It was taking so long to get to the hospital. I whipped out my trusty iPhone and turned on the GPS. Found out that the driver was taking a longer route than what I would have taken. Told the paramedics so and they assured me that the driver knew where he’s going. But of course.
Kim reached earlier than me. His cab was faster than the ambulance.
I arrived at the delivery suite by 230/240pm. It’s all so familiar again…. déjà vu. Seemed like just yesterday I was here; struggling with my first pregnancy.
Settled in; CTG machine on. I text Dr again to let her know I reached.
3pm
Dr came and did all the necessary checks. No dilation. CTG readings seemed ok. No distress signs.
She consulted with us and we all agreed to go ahead with the caesarean today. But my last intake of food was at 2pm and a safer guide will be to do the operation 6 hours after last meal.
Because of placenta previa major, she was undecided if we should go with an epidural or a full-on anaesthesia. The concern is – if the loss of blood was heavy during the caesarean; they would need to transfer me to another theatre and put me on anaesthesia to stop the bleeding.
After consultation with the anaesthetist, we opt for the half body epidural… first.
730pm
Dr came in again and said that we need to wait a while more for the operating theatre to be freed and the anaesthetist to finish up with the last operation.
And so we waited; I waited; Eizac waited.
750pm
Finally! Everyone was ready!
The nurses pushed me down the special passage way and handed over to the OT nurses. Kim was led away to another “secret” waiting area for all the daddies. He wasn’t allowed into the OT because we choose to be in a subsided ward + it was considered an emergency caesarean (again). He was happier this way ‘cos he’s not a huge fan of anything bloody (except medium-rare beef). 🙂
8pm
Though it wasn’t my first caesarean operation, I was still a pack of nerves. There were at least 10 staff buzzing around in the theatre; doing their daily jobs; while I wait like a lamb to be slaughter. Ok; not really. Just almost akin to that. 😛
The anaesthetist was a confident man and called the shots in the theatre. He prepped and started off with the long needle.
One nurse was holding my shoulders to keep me from jerking (it was cold and I was all nerves). Another nurse came over and asked that nurse if she want to go for her break first; she can take over. “NO!” I almost screamed. I asked that 2nd nurse to go away. Leave the first nurse in her position. I can’t guarantee that I won’t move in the midst of the administration of the epidural! Don’t mess with a pregnant woman in the middle of a epidural administration! Grrrggg…..
815 – 830pm
Obstetrician came in her scrubs. Reassured me that she will do her best.
The assistant anaesthetist tested me with an ice pack. This time round, they waited for me to give an all-clear before Dr proceeded with her knife.
During Xi En’s time, I remembered they couldn’t wait for the whole effect of the epidural.
830pm – 850pm
I felt the tugs and nudges. Oh and the familiar coldness of the effect of the epidural.
They tug and pull and pushed. Finally, the anaesthetist (a slightly bigger-built guy) helped to push Baby Eizac from the upper half of my abdomen. Man.. he has some strength!
Wail!!!!!!!! I heard the cries. It’s so relieving to hear him. Dr exclaimed that he’s huge!
The nurses whisked him off for a clean up and checks. But they didn’t bring him back!!!
I thought this time round, I could have a warm fuzzy shot of my newly delivered baby on my chest. Ermm.. not so.
They didn’t tell me what happened. Just said that the doctor was checking him.
9pm
It was taking longer than usual to sew me up. I was staring at the clock and almost dozing off with the calming medicine they pumped into my iv drips.
Subsequently Dr told me that she purposefully waited to see if there were more bleeds before she proceeded with closing me up. Thank God, the bleeds from the placenta weren’t that bad.
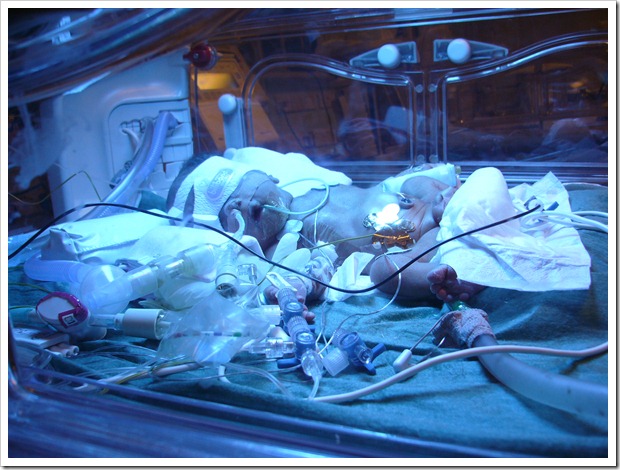
Finally I was done. The nurses came back and told me that Eizac was sent to the Special Care Nursery (SCN) due to some breathing issues. My heart skipped a beat while I was sent to the recovery ward.
920pm
Dr came by to see how I was and told me she will help to go to SCN to check on Eizac.
She came back and reassured me that everything seemed fine. Eizac was opening his eyes and drinking milk while she was there.
It’s probably a transient issue.
950pm
I was sent to the post operating area (POA). It’s not the usual ward as Dr decided to be more careful due to my hyperthyroidism issue coupled with placenta previa major.
Kim came by and told me that he saw baby Eizac.
He’s so cute and round! Of a very healthy weight too – 3.235kg! 51cm.
All was good. They just need to keep him in SCN for a night to observe him further.
31st April 2013
Baby Eizac Chen Kai En – our 2nd precious darling boy – was discharged from SCN.
Both of us were finally in the regular wards.
It’s day 51 today and he went through 6 jaundice and 2 thyroid checks. We were in and out of KKH and the polyclinic throughout Chinese New Year till now.
Finally his prolonged jaundice was cleared up after 1+ month and the doctor gave him an all clear for his thyroid panels as well.
He’s a cute little bundle of joy and I am so happy to celebrate motherhood 2nd time round!